As the number of uninsured individuals rises, counties across the nation are grappling with escalating indigent healthcare costs. Despite these financial pressures, many local governments strive to maintain essential services without compromising quality. The increasing cost of providing healthcare to indigent populations is becoming a major concern, forcing counties to make tough decisions about how to allocate resources while ensuring that vulnerable residents receive necessary medical care.
The Growing Challenge of Indigent Healthcare
Indigent healthcare refers to medical services provided to individuals who lack insurance and sufficient financial resources. Counties are often the primary providers of this care, ensuring that all residents have access to necessary health services. However, the increasing number of uninsured individuals has led to a surge in demand for indigent healthcare, straining county budgets and overwhelming healthcare facilities.
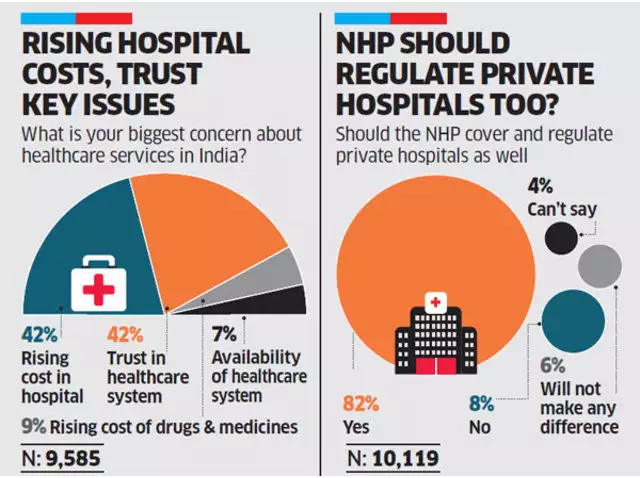
Medical care costs have been rising steadily over the years, outpacing general inflation. Hospitals, clinics, and healthcare providers must navigate a complex landscape of funding, reimbursement rates, and budget limitations. The rising cost of healthcare is attributed to several factors, including higher prescription drug prices, increased hospital expenses, and a growing demand for medical services. As more people seek care without the ability to pay, county governments must absorb the financial burden.
County Responses to Escalating Costs
Despite these challenges, counties remain committed to providing essential health services. Many have implemented programs like the County Indigent Health Care Program (CIHCP), which assists low-income residents who do not qualify for other state or federal healthcare programs. These programs offer a range of services, including hospital care, physician services, and prescription drugs, helping to ensure that vulnerable populations receive the care they need.
To manage costs effectively, some counties have set spending thresholds. Once a county spends a certain percentage of its General Revenue Tax Levy on indigent care, it can request financial reimbursement through state assistance funds. This approach allows counties to maintain some control over their healthcare budgets while continuing to provide necessary services. However, as costs continue to rise, counties may find it increasingly difficult to sustain these programs without additional funding or policy changes at the state and federal levels.
Local governments have also explored alternative funding sources to support indigent healthcare programs. Some counties have turned to grants, partnerships with nonprofit organizations, and increased collaboration with hospitals and healthcare providers. These efforts aim to alleviate some of the financial strain while ensuring that healthcare services remain accessible to those in need.
The Impact on Hospitals and Patients
The financial strain is not limited to county governments; hospitals and healthcare facilities also bear a significant burden. Many hospitals provide emergency care to uninsured patients, often without receiving full compensation for their services. As a result, hospitals experience financial losses that can impact their ability to operate efficiently and provide high-quality care.
In some regions, hospitals have reported substantial increases in costs due to the rising number of indigent patients. This situation has led to budget constraints, staff shortages, and even hospital closures in some cases. When hospitals struggle financially, the entire healthcare system is affected, leading to reduced services, longer wait times, and increased costs for insured patients as hospitals attempt to offset their losses.
Patients are also significantly impacted by the challenges surrounding indigent healthcare. Many uninsured individuals delay or forgo medical care due to cost concerns. Without access to preventive and routine healthcare, these individuals often experience worsening health conditions that require more intensive and expensive treatments down the line. Delayed care can lead to higher hospitalization rates, increased medical complications, and a greater overall burden on the healthcare system.
Additionally, indigent patients often rely on emergency rooms for primary care needs, as they lack access to regular healthcare providers. Emergency rooms are not designed to provide long-term or routine medical care, making them an inefficient and costly option for addressing non-emergency health issues. This pattern contributes to overcrowded emergency departments, longer wait times, and higher operational costs for hospitals.
Looking Ahead: Finding Sustainable Solutions
The challenge of funding indigent healthcare is complex and multifaceted. Counties must balance their budgets while ensuring that vulnerable populations receive necessary medical care. Collaborative efforts between local governments, state agencies, and healthcare providers are essential to developing sustainable solutions that address the root causes of rising healthcare costs and the increasing number of uninsured individuals.
One potential solution involves expanding Medicaid coverage to reduce the number of uninsured residents. States that have expanded Medicaid under the Affordable Care Act (ACA) have seen declines in uninsured rates and reductions in uncompensated care costs for hospitals. Expanding coverage could help alleviate some of the financial burdens on counties and healthcare providers, ensuring that more individuals receive the care they need without overwhelming local resources.
Another approach involves improving access to community health centers and preventive care services. By investing in primary care, mental health services, and early intervention programs, counties can help reduce the need for expensive emergency room visits and hospitalizations. Preventive care plays a crucial role in managing chronic conditions, reducing long-term healthcare costs, and improving overall health outcomes for indigent populations.
Counties may also explore partnerships with nonprofit organizations and private-sector entities to enhance healthcare access and affordability. Community-based initiatives, mobile health clinics, and telemedicine programs can help reach underserved populations and provide cost-effective solutions for delivering care.
As healthcare costs continue to rise, counties will need to advocate for policy changes at the state and federal levels to secure additional funding and resources for indigent healthcare programs. Legislative efforts to control drug prices, regulate hospital charges, and increase funding for safety-net programs could play a vital role in addressing the financial challenges associated with indigent care.
Conclusion
While counties are holding the line amidst skyrocketing indigent healthcare costs, the path forward requires a concerted effort from all stakeholders. The rising cost of healthcare places significant strain on county budgets, hospitals, and patients alike. Addressing this issue will require innovative strategies, increased funding, and policy changes that prioritize the needs of vulnerable populations.
By investing in preventive care, expanding coverage options, and fostering collaboration between public and private entities, counties can work toward a more sustainable healthcare system that ensures access to medical services without overwhelming local resources. The challenge is significant, but with proactive measures and a commitment to finding long-term solutions, counties can continue to provide essential healthcare services while maintaining financial stability.