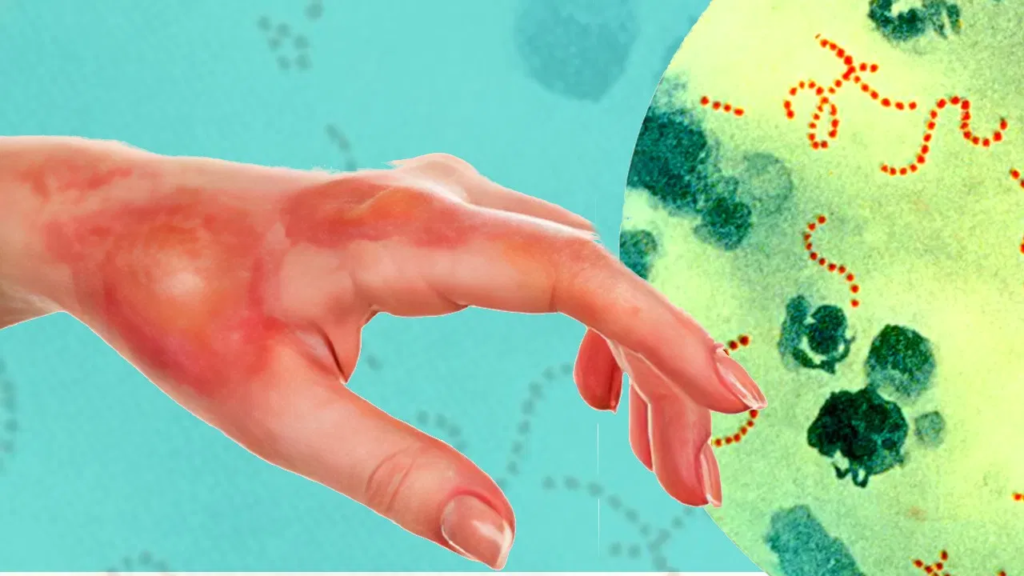
Flesh‑Eating Bacteria outbreak in the USA has claimed several lives and led to a sharp rise in hospitalizations. Public health officials are raising awareness about the dangers of these rare but deadly bacterial infections, particularly during the summer months when people are more likely to swim in warm coastal waters or consume raw seafood.
This article explains what flesh-eating bacteria are, what causes the illness, the symptoms to watch for, how to treat infections, and the most effective ways to protect yourself.
What Are Flesh-Eating Bacteria?
Flesh-eating bacteria refer to harmful microbes that cause necrotizing fasciitis, a serious infection that destroys skin, fat, and tissue covering the muscles. The bacteria enter the body through cuts, scrapes, or other skin injuries and rapidly spread, sometimes within hours.
Several types of bacteria can lead to this condition, including:
- Group A Streptococcus
- Vibrio vulnificus
- Clostridium species
- Escherichia coli (E. coli)
- Aeromonas hydrophila
The most widely reported cases in the USA right now involve Vibrio vulnificus, a bacteria found in warm, brackish waters and raw or undercooked shellfish.
Why Are Cases Rising?
Experts believe the spike in cases is linked to two main factors:
- Rising Sea Temperatures: Climate change is warming coastal waters, creating ideal conditions for Vibrio bacteria to thrive. Regions that previously had few or no cases are now seeing infections, including parts of the Northeast and Midwest.
- More Vulnerable Individuals: People with weakened immune systems, diabetes, liver disease, or cancer are more susceptible to severe infections. As these health conditions become more common, so do complications from flesh-eating bacteria.
In some states, like Florida and Connecticut, health departments have issued alerts due to increased infections during recent heat waves and storm surges.
How Do People Get Infected?
There are two main ways people get infected:
- Through Open Wounds: Bacteria enter the body when open cuts or sores come into contact with contaminated water, such as during swimming, fishing, or walking barefoot on wet sand.
- By Eating Raw Shellfish: Vibrio bacteria can live in oysters and other shellfish. Eating them raw or undercooked can lead to a gastrointestinal infection or, in people with liver disease or other health issues, a bloodstream infection.
Even small wounds like blisters, insect bites, or new tattoos can act as entry points for bacteria.
Symptoms to Watch For
Symptoms can appear quickly—within hours of exposure—and worsen rapidly. Early recognition is key to survival.
Common symptoms include:
- Severe pain near the wound site
- Swelling, redness, or warmth
- Blisters or black spots on the skin
- Fever and chills
- Fatigue and confusion
- Vomiting or diarrhea (especially after eating seafood)
If left untreated, the infection can spread to the bloodstream and lead to sepsis, organ failure, or death.
How Deadly Is It?
Flesh-eating bacterial infections are rare, but when they occur, they are extremely serious. According to health data:
- The mortality rate ranges from 20% to 35% depending on the speed of treatment and the individual’s health condition.
- For Vibrio vulnificus bloodstream infections, the fatality rate can reach 50%.
Prompt diagnosis and immediate treatment are essential to improve survival chances.
Treatment Options
Treatment for necrotizing fasciitis and Vibrio infections must begin urgently. Delays can be fatal.
The standard treatment includes:
- Intravenous Antibiotics: A mix of strong antibiotics is given through an IV to stop the spread.
- Surgical Debridement: Infected tissue must often be surgically removed. Multiple surgeries may be needed.
- Supportive Care: In severe cases, patients require care in an intensive care unit (ICU), including breathing assistance and fluid replacement.
In some instances, doctors may need to amputate a limb to save the patient’s life. Even with aggressive care, some patients suffer long-term effects such as disfigurement, mobility loss, or emotional trauma.
Who Is Most at Risk?
While anyone can get infected, some groups are at higher risk:
- People with chronic health problems like diabetes, kidney disease, or cancer
- Individuals with liver conditions such as hepatitis or cirrhosis
- Those who are immunocompromised due to medications or medical conditions
- Elderly adults, especially those over age 65
- People with recent surgery, tattoos, or skin injuries
- Consumers of raw oysters or shellfish
These groups should take extra care when near warm waters or handling seafood.
How to Protect Yourself
Preventing flesh-eating bacterial infections is possible with some simple safety steps.
For water exposure:
- Avoid swimming in warm saltwater or brackish water with open wounds.
- Cover cuts, scrapes, or recent piercings with waterproof bandages.
- Rinse thoroughly after swimming or fishing, especially if you have minor skin injuries.
- Shower promptly after beach or lake visits.
For seafood safety:
- Cook all shellfish thoroughly. Do not eat raw oysters or clams, especially during warm months.
- Wear gloves when handling raw seafood.
- Clean kitchen surfaces and utensils after preparing seafood.
For wound care:
- Clean all wounds with soap and water immediately.
- Apply antiseptic and keep the wound covered until it heals.
- Watch for unusual redness, pain, or swelling around the injury.
If you feel unwell after exposure to water or seafood, or if a wound worsens quickly, seek emergency care right away.
What Is the Government Doing?
State and federal health agencies are monitoring outbreaks and issuing warnings. The Centers for Disease Control and Prevention (CDC) advises hospitals and clinics to stay alert for symptoms and act quickly when cases are suspected.
Local health departments in coastal states have placed public notices at beaches and piers warning about the risks, particularly for immunocompromised people and those with open wounds.
Some regions are even considering issuing Vibrio forecasts—similar to pollen or UV alerts—during peak risk seasons.
Public Awareness Is Key
Doctors and health experts stress that while these infections are rare, public education is essential. Many people ignore early signs or think they have a minor injury. But in these cases, time lost is life lost.
The public is encouraged to:
- Stay informed about local health alerts
- Avoid risky behavior when vulnerable
- Talk to doctors about individual risk levels, especially if they have pre-existing health conditions
In some recent fatal cases, patients delayed going to the hospital for more than 24 hours, thinking they had a muscle strain or minor skin irritation. Unfortunately, that delay often makes the difference between life and death.
Conclusion
The flesh-eating bacteria outbreak in the USA is a reminder of how fast and dangerous certain infections can be, especially when environmental and health conditions align. The rise in cases may continue if climate trends persist, putting more people at risk.
Knowing how these bacteria spread, recognizing early symptoms, and acting quickly are the best defenses. Whether you’re going to the beach, eating seafood, or recovering from surgery, a few precautions can go a long way.
Do follow on Instagram
Also Read : 10 Best Fashion Trends in the USA Right Now