In recent years, the United States has faced a sobering reality: veteran suicide rates are alarmingly high, Medicare with an average of 17.6 veterans taking their own lives each day, according to the Department of Veterans Affairs (VA). Suicide remains the second-leading cause of death among veterans under 45, a statistic that underscores the urgent need for comprehensive mental health support. In response, Medicare has announced expanded mental health coverage aimed at addressing this crisis, particularly for veterans who rely on its services. This move is part of a broader effort to enhance access to care, reduce barriers, and provide critical resources to those struggling with mental health challenges.
The Veteran Suicide Crisis: A Growing Concern
Veterans face unique mental health challenges, often stemming from their military service. Post-traumatic stress disorder (PTSD), depression, anxiety, and traumatic brain injuries (TBI) are prevalent among this population, contributing to elevated suicide rates. According to a 2021 report, Alabama’s veterans experienced a suicide rate of 35.4 per 100,000, surpassing both the national veteran average and the state’s general population rate. Transgender veterans face even higher risks, with studies indicating they are twice as likely to die by suicide compared to cisgender veterans and nearly six times more likely than the general U.S. population. These numbers paint a stark picture of a community in need of robust, accessible mental health care.
The VA has long been a cornerstone of veteran healthcare, providing services to over nine million veterans nationwide. However, challenges such as long wait times, staffing shortages, and restrictive policies have hindered its ability to meet the growing demand for mental health support. Recent reports indicate that veterans can face waits of up to four months for mental health appointments, a delay that can be life-threatening for those in crisis. Medicare’s expanded coverage aims to bridge these gaps, offering veterans additional pathways to care and complementing VA efforts.
Medicare’s Expanded Mental Health Coverage
In 2025, Medicare introduced significant changes to its mental health coverage to better serve veterans and other beneficiaries. These changes include increased access to telehealth services, expanded provider networks, and coverage for a wider range of mental health treatments, such as therapy, counseling, and peer support programs. The goal is to ensure that veterans, particularly those in rural or underserved areas, can access timely care without the barriers of long wait times or limited provider availability.
Telehealth has emerged as a critical tool in this expansion. The VA has been a pioneer in virtual healthcare for over two decades, using telehealth to reach veterans in remote areas. Medicare’s new policies build on this foundation, covering virtual therapy sessions and consultations with mental health professionals. This is especially vital for veterans who may struggle with transportation or live far from VA facilities. By integrating telehealth into its coverage, Medicare is making it easier for veterans to connect with counselors, psychologists, and psychiatrists from the comfort of their homes.
Additionally, Medicare is expanding its provider network to include more mental health specialists, such as licensed clinical social workers and marriage and family therapists. This move addresses the shortage of mental health professionals within the VA system, where staffing cuts and return-to-office mandates have strained service delivery. By allowing veterans to seek care from a broader pool of providers, Medicare is reducing the burden on VA facilities and ensuring more timely access to care.

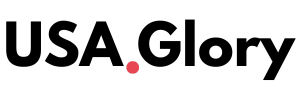
Addressing Barriers to Care
One of the most significant barriers to mental health care for veterans is the stigma surrounding mental health issues. Many veterans hesitate to seek help due to fears of being perceived as weak or concerns about confidentiality. Medicare’s expanded coverage includes initiatives to promote peer support programs, which connect veterans with others who have shared experiences. These programs, often facilitated by community-based organizations, create safe spaces for veterans to discuss their challenges and access resources without judgment.
Another critical issue is the VA’s strict requirements for families seeking death benefits after a veteran’s suicide. A CNN investigation revealed that the VA has denied hundreds of claims from families because veterans did not have documented mental health diagnoses linked to their service. Medicare’s expanded coverage aims to prevent such tragedies by ensuring veterans can access care before reaching a crisis point, potentially reducing the number of families left to navigate these complex claims processes.
The expansion also addresses specific needs within the veteran community, such as postpartum and perinatal mental health for women veterans, who are the fastest-growing group using VA services. Programs focused on health during and after pregnancy aim to tackle postpartum depression and related concerns, offering tailored support to this vulnerable population.
Community-Based Solutions and Funding
To complement Medicare’s efforts, the VA has announced $52.5 million in grants for community-based organizations to develop suicide prevention and emergency clinical service programs. These grants, awarded through the Staff Sgt. Parker Gordon Fox Suicide Prevention Grant Program, support initiatives like wellness checks, training enhancements, and mental health tools tailored to veterans’ needs. Since its launch in 2022, the program has distributed $157.5 million to 95 organizations across 43 states, territories, and tribal lands, demonstrating a commitment to community-driven solutions.
Organizations like American Veterans are also stepping up, conducting awareness campaigns to highlight available resources. Their recent eight-city tour aimed to connect veterans with local services and reduce feelings of isolation, emphasizing that no veteran should feel alone in their struggles. These grassroots efforts, combined with Medicare’s expanded coverage, create a multi-faceted approach to tackling the suicide crisis.
Challenges and Criticisms
Despite these advancements, challenges remain. Recent policy changes, including return-to-office mandates for VA mental health providers, have sparked concerns about reduced access to telehealth services. Many providers hired for remote positions are now required to work from offices that may lack private spaces for confidential sessions, potentially compromising care quality. Additionally, staffing cuts at VA facilities have led to longer wait times, with some veterans waiting up to 45 days for appointments. These issues highlight the need for careful implementation of new policies to avoid undermining progress in mental health care.
Critics also point to proposed federal budget cuts that could impact mental health services. For example, a leaked proposal to defund specialized 988 Suicide & Crisis Lifeline services for high-risk groups, including veterans, has raised alarms among advocates. The 988 hotline provides immediate access to trained counselors, and any reduction in funding could limit its effectiveness for veterans in crisis.
A Path Forward
Medicare’s expanded mental health coverage is a promising step toward addressing the veteran suicide crisis, but it must be part of a broader, coordinated effort. Collaboration between Medicare, the VA, and community organizations is essential to ensure that veterans receive the care they need when they need it. Initiatives like Alabama’s veteran mental health plan, which focuses on crisis care, treatment access, and suicide prevention, serve as a model for other states. By prioritizing partnerships and innovative programs, policymakers can create a more resilient support system for veterans.
For veterans and their families, the message is clear: help is available, and no one should face their struggles alone. The 988 Suicide & Crisis Lifeline remains a critical resource, offering immediate support for those in distress. Veterans can also access VA services, community programs, and now, expanded Medicare coverage to find the care that best fits their needs.
As the nation continues to grapple with the veteran suicide crisis, Medicare’s commitment to expanding mental health coverage offers hope. By addressing barriers, increasing access, and supporting community-driven solutions, this initiative aims to save lives and honor the sacrifices of those who have served. For veterans struggling with mental health challenges, these changes signal a renewed focus on their well-being, with the promise of a brighter, more supported future.
Also Know :- Dow Surges 740 Points on Eased Trade Tensions, Marking Best Day in 2025